A new study shows that screening for prostate cancer doesn’t necessarily save lives
Prostate cancer screening is about to get a whole lot cloudier.
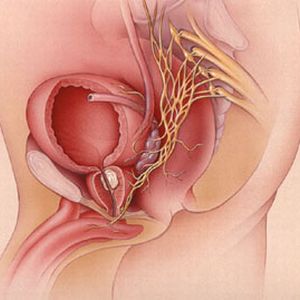
Published this morning in the NEJM, the results of the study by the National Cancer Institute showed that, for men who were screened with both a PSA and digital rectal exam, there was no difference when compared to men who received “usual care.”

The results confirm the suspicions that many physicians already had, namely, that screening for prostate cancer does not appear to save lives.
As I have written countless times, there are many other diseases that can raise a PSA level. Combined with the fact that physicians have to act on elevated levels, this can lead to excessive prostate biopsies, as well as treating early cancers that end up not being the ultimate cause of death. All of these procedures expose the patient to a host of side effects, including bleeding and infection from the biopsy, and impotence and urinary incontinence from prostate cancer treatment.
The study was paired with the findings from a concurrent European study, which was not quite as negative. Nonetheless, the benefit of prostate cancer screening was minimal, with “7 fewer prostate cancer deaths for every 10,000 men screened and followed for nine years.”
Already, the USPSTF is shying away from endorsing prostate cancer screening by updating their guidelines last year, no longer recommending a PSA test for men older than 75.
So, what to do if you’re a patient? I think it’s more imperative than ever not to accept the dogma that “more screening is better medicine.” If anything, the decision of obtaining a PSA test needs to be thoroughly discussed with your doctor. Suddenly, the benefits of going down the path of screening doesn’t necessarily outweigh the risks.
Many may find that counterintuitive, and to be honest, it’s a hard truth to swallow. But these findings can help counter the pervading myth that obtaining every conceivable screening test is a sure way to improve health, when in actuality, it isn’t.
